In Sonoma County since the surge of COVID-19 cases in late June, our senior congregate living homes have consistently had about 82% of the fatalities in our county. This fact is consistently reported in our media on a weekly basis. Early on in this outbreak, the term “die offs” was commonly used in facilities in recognition of how quickly some of our residents died after onset of COVID. As in many other areas in our country, the initial bad outcomes were associated with the lack of PPE and timely testing, as well as staff shortages, and the need to learn and practice optimal IPC (Infection Prevention and Control). However, with the in-facility assistance of specialists from CDPH HAI (Health Associated Infection) program, HSAG QIO (Health Services Advisory Group), and our public health department, most of our facilities have extinguished their initial outbreaks and have minimized the impact of new cases.
This means most of our facilities are able to accept new admissions including transfers from our acute hospital partners for post-acute rehab. These referrals have slowed to a trickle in part due to public fear about the high risk of acquiring COVID and dying, should they enter our facilities. Case managers have told us their LOS has increased as patients and families attempt to improve sufficient for discharge to the home setting.
Is this fear still justified?
In my county, the mortality in ALFs (Assisted living facilities) is reported with SNF mortality adding up to the 82% mortality, yet the ALFs operates by a social model which usually have much less robust IPC capacity than SNFs.
In our county, we spent March through June preparing for a surge with emphasis on ACP (Advance Care Planning) and palliative care in our work groups. Many of our high risk residents did choose to avoid hospitalizations in favor of on-site palliative care. These patient centered care actions likely contributed to our higher mortality. Our media though hasn’t reported these reasons for our higher mortality. Our mortality may also be much higher than that of independent living seniors because our resident population is frailer, less functional, and has more advanced and serious medical conditions. Traditionally, the average life expectancy of our custodial patients has been about 2.5 years.
 At a recent meeting convened on behalf of seniors by one of our county supervisors, I suggested the public would be well serviced if our public health department reviewed the deaths in our senior congregate living facilities to see how many occurred in long stay (>100 days) residents or those on Hospice. Our public health officer agreed to look into this, but I’ve not yet seen their report.
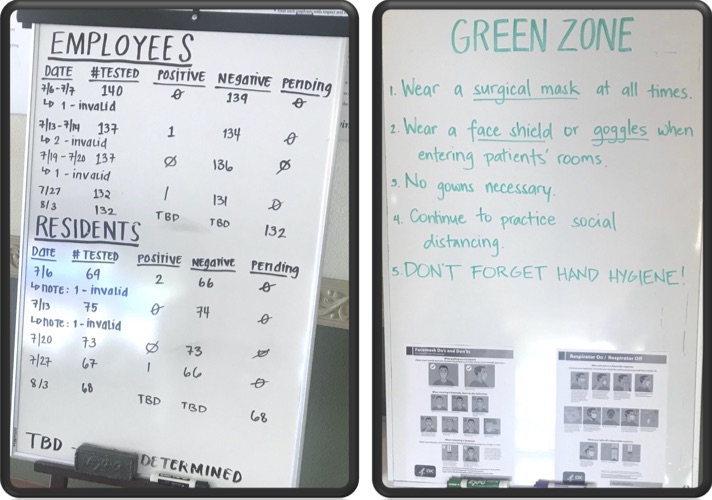
At a recent meeting convened on behalf of seniors by one of our county supervisors, I suggested the public would be well serviced if our public health department reviewed the deaths in our senior congregate living facilities to see how many occurred in long stay (>100 days) residents or those on Hospice. Our public health officer agreed to look into this, but I’ve not yet seen their report.I shared this information with our incoming CALTCM President, Dr. Albert Lam, and he shared another valuable approach to quieting staff and public fears. He recommends each facility enhance their public transparency. He shared these 2 photos of messaging actions one of his facilities has produced (photos shared with permission).
This once in a century pandemic has disrupted our communities and caused many to live in “paralyzing fear”. One of our obligations is to help our communities minimize the prevalence of COVID, and make wise and informed choices.


Thank you Dr. Gieseke. As an Executive Director at a SNF, I appreciate your accurate opinion on this subject.