| 2017 INTERACT Null Findings |
|
by Albert Lam, MD A new study from the Interventions to Reduce Acute Care Transfers (INTERACT) team at Florida Atlantic University appears to cast doubt on the ability of INTERACT to reduce readmission rates. The study, published in the Journal of the American Medical Association Internal Medicine, showed no significant reduction in overall hospital admissions (per 1000 resident-days) in the intervention group that received INTERACT training and no difference in 30-day readmissions or ED visits compared to facilities that did not receive INTERACT training. These findings are striking, and bring into question the effectiveness of INTERACT in reducing nursing facility to hospital readmissions. Yet, despite all of this, our own experience is that INTERACT makes an incredible difference in nursing facilities. So what does this really mean? To answer this question, it helps to know a little about the history of INTERACT. In 2009, the INTERACT program studied 30 non-randomized volunteer nursing homes over 6 months and found a 24% reduction in all-cause hospitalizations among actively participating nursing homes versus a 6% reduction for nursing homes that were not actively participating. Overall hospital admission reduction was 17%. These remarkable findings, published in 2011, subsequently led to wide adoption of INTERACT in nursing homes across the United States. In 2013-2014, the INTERACT team sought to further study the effects of their program in a randomized facility-level trial with some facilities receiving INTERACT training and implementation support. This randomized trial provided a more robust way to compare intervention facilities versus non-intervention facilities, and the study authors hypothesized that those facilities with the INTERACT training and implementation support would have greater reduction in rates of hospitalization and ED visits than control nursing homes. For this study, 33 intervention facilities and 52 non-intervention facilities that had no prior INTERACT use were included in the experimental and control groups, respectively. The findings bring us back to the beginning of this article: no statistically significant difference on hospitalizations or ED visit rates. For any facilities wondering about whether INTERACT will be effective at lowering your readmission rates, there are 3 critical questions to consider: 1. Is your readmission rate already low? This study was conservatively designed, making it difficult to reach statistical significance unless a large improvement of greater than 6.5% occurred. Any nursing facility improvement less than 6.5% would not be large enough to reach statistical significance in this study, so facilities with baseline readmission rates < 10% were excluded from this study to help improve the chances of catching improvements. In five out of the six measures used, both the intervention and control groups improved, but the difference between the intervention and non-intervention facilities was not large enough to reach statistical significance. The take-home point here is that the online and telephonic training and implementation of INTERACT was not statistically better than what the non-intervention facilities did during the same time. 2. What were the improvements made by non-intervention nursing facilities? This study’s intent-to-treat analysis means that even “non-intervention” facilities could have implemented INTERACT-type interventions during the active study period after the facilities were randomized to their groups.
While not described in the study, the widespread use of SBAR communication and increased focus on improved assessments by nursing facilities, hospitals, and medical groups may mean that participating SNF readmission rates have already made improvements. Other tools like STOP-AND-WATCH may have also been implemented in nursing facilities that did not receive INTERACT training. At the time of the data collection in 2013-2014, the Hospital Readmission Reduction Program with its penalties for excessive readmissions for certain diagnoses was already underway nationally, so many facilities were already making some efforts to reduce rehospitalizations. Against this background, it is possible that implementation of INTERACT in this training, simply did not impact the readmission rates enough to reach statistical significance. A nursing facility that is doing only part of INTERACT but believes they are already reaping many of the benefits can look for assurance if they hold frequent, regular SBAR reviews with active discussions from multiple team members about opportunities for improvement. This type of teamwork is critical to succeed with INTERACT and is a focus of CALTCM’s SNF 2.0® program, and it brings us to our last question. 3. How committed is your facility to performing and sustaining quality assessment, performance improvement (QAPI) activity around INTERACT? Your nursing facility’s answer to this question will determine the degree of your success with INTERACT. One of the potential weaknesses in the study was using a training and implementation regimen that relied on online training and telephonic support. While online and telephonic support offers improved access to training compared to no training, the results of this study suggest that this “INTERACT-lite” type of intervention may not provide the nursing facilities sufficient mentorship and guidance to more fully implement and sustain INTERACT activity. In our experience with CALTCM SNF 2.0® mentorship, a personal connection offers depth of support and engagement with staff that provides the necessary boost SNFs need to implement INTERACT as a QAPI program. Commitment to QAPI activity around INTERACT helps teams learn together, work together, and find success together. Given the high staff turnover that occurs in many SNFs, regular QAPI activity also helps new staff to quickly engage and adopt quality care practices, thereby sustaining successful INTERACT practices. In conclusion, this new INTERACT study did not show statistically significant improvements in hospitalizations or emergency room use for INTERACT intervention facilities compared to non-intervention facilities. Trends toward improvement suggest that INTERACT intervention may help reduce hospitalizations, but the inability to break away and show a statistically significant difference may signal areas of weakness in this study’s INTERACT implementation practice. Many current INTERACT implementation practices may be similarly limited. This should cause nursing facilities to pause and evaluate their own INTERACT implementations. Certainly intuitively, even if not statistically, the more robustly a facility embraces INTERACT and QAPI, the higher the probability of excellent care, and the lower the probability of inappropriate rehospitalizations. About CALTCM SNF 2.0® CALTCM SNF 2.0® focuses on bringing facilities the most effective approach to implementing INTERACT. Through the almost 50 facilities we’ve trained in SNF 2.0®, we have found that onsite mentorship is more effective with facility-specific problem solving and offers facilities more accountability as they adopt INTERACT. This study, however, relied upon webinar and telephonic interventions that may have limited the program’s effectiveness and ability to provide problem solving guidance and accountability. CALTCM SNF 2.0® is designed to address real-world implementation barriers and augments nursing facility INTERACT programs with a tailored, hands-on approach to leadership training and mentorship and cross-continuum systems-based approach to care partnership. It was piloted in 2 facilities in 2013 and resulted in a 33-66% reduction in 30-day readmission rates sustained over 12 months and has since expanded to more than 40 facilities in 2016 as a part mentor, part telephonic coaching program. Analysis for the latest effort is ongoing. 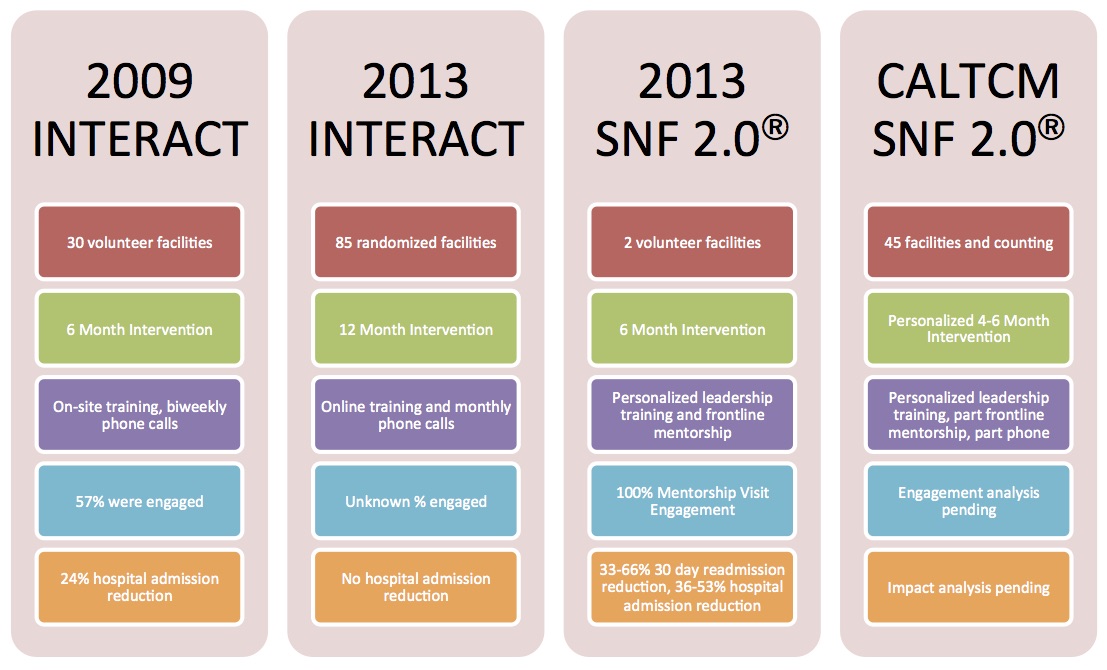 |

